How MRI-Guided Ultrasound Can Help Detect Prostate Cancer
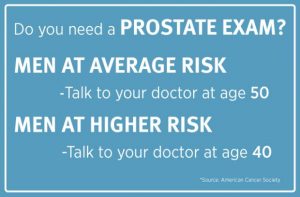
As many as 1 in 6 men will get prostate cancer. That makes it the most common type of cancer for men after skin cancer. When it comes to testing, the American Urological Association says the greatest benefit of screening appears to be in men ages 55 to 69 years. But Dr. Todd Brandt of Metro Urology in St. Paul, Minnesota says it’s not a young man’s or an old man’s disease. Instead, all men need to be aware of risk factors and familiar with the tests that help detect prostate cancer.
Most Common Prostate Exams
The most common prostate screening exams are 1.) a blood test that checks your PSA level and 2.) a rectal exam. Unless either of these point to a problem, or you’re having symptoms like difficulty going to the bathroom, the PSA and the rectal exam are likely all you’ll ever have. But, if you have an abnormal exam or cancer is detected, you can expect a biopsy. The industry standard is a transrectal ultrasound (called TRUS) biopsy performed in your urologist’s office. Dr. Brandt says the TRUS biopsy does have shortfalls. In some patients, a biopsy is negative but their PSA level is still rising. It may mean the ultrasound didn’t see the cancer. Dr. Sidney Walker, a body radiologist at RAYUS, says a TRUS biopsy isn’t always able to identify the prostate cancer because of where the cancer lesion is located. There’s actually a region of your prostate that is hard to see with ultrasound says Dr. Brandt:
“An ultrasound isn’t necessarily all that sensitive for picking up areas or specific parts of the prostate or zones of the prostate which may harbor the cancer. That is, we can look with an ultrasound but we may not actually see the cancer.”
“Seeing the Cancer” with MRI-Guided Ultrasound
Today, urologists like Dr. Brandt are starting to use MRI as a tool to better “see” the cancer. So after your PSA and rectal exam, if something is detected, your doctor may send you for an MRI. If a suspicious area is identified, knowing exactly where it is can help target the next biopsy. The images from the MRI are actually used during the ultrasound biopsy as a sort of a map. One way this is done uses Prostate MRI and ultrasound together – called TRUS fusion, this new technique fuses the two types of technology.
With the TRUS fusion technique, the urologist can take an MRI image and overlay it on to their TRUS ultrasound system. The fusion technique couples real-time ultrasound with images from an MRI to help target the areas within the prostate that are suspicious to the radiologist. Dr. Brandt explains the steps:
- You get an MRI
- The MRI images are read by a radiologist who outlines suspicious areas
- The MRI images are sent electronically to your urologist
- The urologist loads the images into software
- During your ultrasound, real-time ultrasound images are paired with the MRI images to guide the doctor to a very specific area
In his office, Dr. Brandt tells his patients with an elevated PSA or an abnormal exam, “If we want to get the best, most accurate biopsy that we can these days, we’ll use an MRI ahead of doing an ultrasound-guided biopsy to accurately target any areas that are suspicious.”
Back in 2006 when Dr. Walker first started reading prostate MRIs, they were being used to help the oncologist plan radiation therapy. A decade later he’s using MRI images to guide urologists in TRUS biopsies. For a patient, that means your first stop after a PSA, rectal exam and TRUS biopsy could be an MR machine.
What to Expect from a Prostate MRI
It’s always nice to know what your exam is going to be like before you arrive for your appointment. When it comes to getting a Prostate MRI, you can expect to be lying on your back on a table that slides into the machine containing a powerful magnet. The exam typically takes 30 to 45 minutes. Depending on where you schedule your exam, you may have an endorectal or body coil. Asking about the coil is a good question when you book your appointment. Keep in mind, this scan can be very valuable in your care and treatment. “MRI is actually able to identify cancers that we’re not seeing during the ultrasound examination,” says Dr. Walker.
Changing Standard of Care?
Will a Prostate MRI eventually become the standard of care? Dr. Walker thinks so. Across the country and in the minds of urologists, he says the Prostate MRI is becoming essential for the management of patients at risk of prostate cancer.
“Now I think a lot of docs are becoming more comfortable using the MRI ahead of time to get a little bit more accurate biopsy. And more patients actually know about the MRI technology and even ask about it.” -Dr. Todd Brandt of Metro Urology